Blog
ADAA Fall Forum: Sex and Anxiety
This webinar discusses sexual anxiety and interventions for the most frequently encountered sexual dysfunction in women and men.
Read MoreThe Uses of Virtual Reality in Social Anxiety Treatment
Dr. Rosen and Dr. Spinner recently presented a session on The Uses of Virtual Reality in Social Anxiety Treatment for the National Social Anxiety Center. View the presentation on The Uses of Virtual Reality in Social Anxiety Treatment. We Can Help If you are experiencing social anxiety or would like...
Read MoreIs Exercise A Viable Treatment For Depression?
Exercise has long been viewed as being beneficial for physical health, but in recent years there has been increasing interest in using it as an effective, natural treatment option for mental health issues like depression. I have noticed that many people who seek treatment in our clinic aren’t aware that...
Read MoreThe Growing Childhood Obesity Epidemic
Growing up in the United States, many of us enjoyed a childhood filled with fun and games. Whether it was playing tag on the playground or challenging our friends at sports competitions, we had an abundance of energy that frequently seemed inexhaustible. Today, however, that is often not the case,...
Read MoreJerome Siegmeister, MD, MaED – Consult The Expert On Why You Can’t Focus
Lately, likely due to the increased coverage on television and in social media, many people have been coming in to see me saying they have poor attention, they can’t focus, and they think they may have ADHD. Some do, some don’t. When they do have it, the best treatment often...
Read MoreHow To Reduce Holiday Stress
The holidays are a time to enjoy family, friends, and good cheer, but as we go through this joyous season, many of us struggle with mental health challenges and stress due to a combination of social obligations, financial burdens, and other factors. From going to festive events we may have...
Read MoreSeth Grobman, Psy.D. – Consult The Expert On Telehealth Visits
For this month’s Consult The Expert interview, I spoke with Seth Grobman, Psy.D., a clinical psychologist here at The Anxiety Center. Dr. Grobman has been practicing traditionally for more than twenty years. When the covid pandemic hit, he pivoted to telehealth so he could continue to treat patients during the...
Read MoreAndrew Rosen, PhD, ABPP, FAACP – Consult The Expert On The Dangers Of The Media And Outside Influencers
For this month’s Consult The Expert interview, we talked with Dr. Andrew Rosen, the founder of The Center for Treatment of Anxiety and Mood Disorders. Dr. Rosen has been a practicing clinician for over forty years, so he is well-versed in the changes that have taken place regarding mental health...
Read MoreBrittany Schulman, Psy.D – Consult The Expert On ADHD
This month, I spoke with Brittany Schulman, Psy.D for our Consult The Expert interview. She’s a licensed clinical psychologist here at the Center and has a special interest in diagnosing and treating Attention Deficit/Hyperactivity Disorder (ADHD). Most of us have at least a vague understanding of ADHD, but may not...
Read MoreVanessa Finkelman, Psy.D – Consult The Expert On Social Anxiety
This month, I talked with Vanessa Finkelman, Psy.D. As a postdoctoral fellow, she will be treating various anxieties and mood disorders at our center, beginning in September. One of her special interests is in working with those who are challenged by social anxiety, which is the fear of being judged...
Read MoreBump or monkeypox, cough or COVID-19: Am I seriously sick or am I living in 2022?
Fever, chills, bumps, rashes, sore throat, sniffles, headache, oh my – could having any of these symptoms mean you might be seriously ill?
Read MoreEric Spinner, Psy.D – Consult The Expert On Eating Disorders
This month, we talked with Eric Spinner, Psy.D. Beginning in September, he will be working at The Center for Anxiety and Mood Disorders as a Post Doctoral Resident. For the past two years before joining the team, Dr. Spinner worked at a residential facility for women, treating adolescents to older...
Read MoreDoes Anxiety Get Better With Age?
It’s no secret that the elderly population is the fastest growing age group in the United States. In fact, there are now approximately 76 million baby boomers in the United States and that number is increasing daily. While some things get better with age (think of fine wines), will aging...
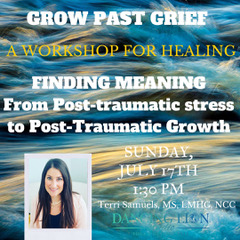
Read MoreFinding Meaning: From Post-traumatic stress to Post-traumatic Growth
May is Mental Health Awareness Month. At Dancing Lion Studio we are dedicated to bring you the best in not only yoga, meditation and movement, but all the healing arts. Beginning this summer we will be offering a wide variety of workshops lead by professionals who’s ideals are in alignment with...
Read MoreDarbi Miller, MS, LMFT – Consult The Expert On Increasing Relational Self-Awareness
For this month’s Consult The Expert interview, we spoke with Darbi Miller, MS, LMFT, one of the marriage and family therapists here at The Center For Treatment Of Mood And Anxiety Disorders. Although she likes working with all ages, she enjoys the dynamic surrounding family and relationships.
Read MorePost-Pandemic Social Anxiety: Simple Steps To Start Living Again After Covid
My colleagues and I have noticed a dramatic increase in anxiety and anxiety-related disorders over the past two pandemic years. While apprehension is a typical response during times of strife, as we return to more normal lives, many people have been caught off-guard to realize how uncomfortable they now are...
Read MoreLonette Belizaire, Ph.D. – Consult The Expert On Cognitive Behavioral Therapy (CBT) And Self-Care
Dr. Lonette Belizaire works with young adults in our Anxiety Center, as well as with children and teens in our Children’s Center. Her primary treatment approach utilizes cognitive behavioral therapy (CBT). This is a modality which helps people recognize and change their negative thoughts and behaviors. Cognitive behavioral therapy can...
Read MoreNonie L. Craige, LCSW – Consult The Expert On Communication And Relationships
In our second Consult The Expert interview for March, we spoke with Nonie L. Craige, LCSW, a psychotherapist at the Center for Treatment of Anxiety and Mood Disorders.
Read MoreCovid Stress And The Pandemic’s Effects On Society: A Psychologist’s Observations
As a psychologist who treats anxiety daily, I’ve been in a unique position during the pandemic. I can distinctly see the difference the last two years have had on individuals, families, and society in general.
Read More